The idea behind IVF is that, by removing several of the variables encountered during the initial steps of reproduction, the overall chance of pregnancy is increased. IVF has become so successful that pregnancy rates now surpass those associated with traditional reproduction. Whereas a healthy fertile couple has a 20-25% chance of conceiving every month, good prognosis infertility patients have a 40-50% chance of pregnancy with a single IVF cycle.
indications
IVF was originally developed for women with nonfunctioning fallopian tubes (tubal factor). With the development of improved clinical protocols and new laboratory techniques (such as ICSI), the indications for IVF have expanded over the years and, in 2007, there were more than 132,000 cycles performed in the United States. Current indications for IVF include:
Tubal Factor
Male Factor
Uterine Factor
Premature Ovarian Failure
Ovulatory Dysfunction
Endometriosis
Diminished Ovarian Reserve
Unexplained Infertility
clinical protocol
IVF is a complex process with subtle variations in approach. At Napa Valley Fertility Center, each IVF cycle is individually tailored to optimize your outcome. We are continuously refining our protocols and adding new treatment adjuncts in an effort to improve your chances for pregnancy.
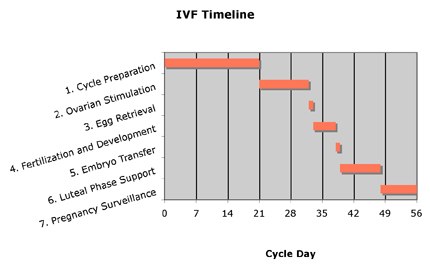
A typical IVF cycle consists of 7 steps and takes roughly 6-8 weeks to complete. The following narrative explains each of these steps, noted in the chart below, in detail.
-
Step 1. Cycle Preparation
-
Once a decision to proceed with IVF is made, a series of evaluations must be completed prior to initiating therapy. These include:
-
1)Infectious disease testing (blood work) for both the male and female.
-
2)An imaging study of the uterine cavity.
-
‣Saline infusion sonogram (SIS)
-
or
-
‣Hysterosalpingogram (HSG)
-
To prevent any unwanted ovarian activity from occurring during the IVF cycle, it is also during this preparatory time that medications such as birth control pills and/or Lupron are often started.
-
Step 2. Ovarian Stimulation and Follicular Monitoring
-
The goal of ovarian stimulation is to promote the development of as many oocytes (eggs) as possible. Because not every fertilized egg ultimately results in a baby, working with a surplus of oocytes increases your overall chance of success. Multiple egg development is accomplished through the use of medications called FSH and LH, collectively known as gonadotropins (Trade names: Gonal-F, Follistim, Menopur, Luveris). These are the same hormones that your brain produces during a normal menstrual cycle to promote a single ovulation.
-
-
Step 2 begins with an evaluation of your ovaries to assess their readiness to undergo stimulation and consists of the following two tests:
-
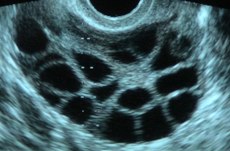
‣Ultrasound: An imaging study that allows visualization of the millimeter-size ovarian follicles (the fluid filled cysts which each contain a single egg).
-
‣Estradiol (E2): A hormone whose blood level reflects ovarian activity.
-
If the ovaries show no activity, you may begin taking medication. After 4-5 days of stimulation, another ultrasound and E2 will be performed and this pattern continues every 1-2 days until the majority of follicles have reached their full growth potential (usually around 16-20 mm in diameter). To accomplish this, the average patient receives a total of 10-12 days of medication.
-
-
In preparation for oocyte retrieval, one final injection of a medication called hCG (Trade names: Pregnyl, Novarel, Profasi, Ovidrel) signals your eggs to undergo the final maturation process. hCG is administered at night and, approximately 36 hours later, you will have your egg retrieval.
-
Step 3. Oocyte (Egg) Retrieval
-
Egg retrieval is a minimally invasive outpatient surgical procedure. Under direct ultrasound visualization, a special needle is used to aspirate fluid from the mature ovarian follicles. As fluid is removed from the follicles, it is passed to the embryologist in the laboratory where it is examined for the presence of an egg. Oocytes are then isolated in Petri dishes and placed into an incubator.
-
-
The recovery period after the procedure lasts for 1-2 hours in the office and this is followed by a period of modified bed rest at home for an additional 1-2 days.
-
Step 4. Fertilization and Early Development
-
Fertilization of the eggs takes place the same day as the retrieval and is accomplished by one of the following techniques:
-
‣Conventional insemination: A single egg is incubated in the presence of 100,000’s of sperm.
-
‣ICSI (Intracytoplasmic sperm injection): A single sperm head is injected directly into a single egg.
-
-
Which fertilization method used will depend upon your specific medical diagnosis.
-
-
On the morning after the retrieval, your eggs will be evaluated for fertilization. Typically, fertilization will be successful for 2/3 of the group and these single cells are now referred to as zygotes. By the second day after retrieval the conceptus is now called a pre-embryo and consists of 2 to 4 cells.
-
Step 5. Embryo Transfer
-
Depending upon the outcome of your cycle, embryos will be returned to your uterus on either day 3 or day 5 after the egg retrieval. Dr. Uzelac will discuss with you the latest information from the lab about the quality of your embryos. Based on ASRM guidelines, Dr. Uzelac and you (and your partner) will agree about the number of embryos to be placed in your uterus.
-
-
The embryo transfer takes place under ultrasound guidance and does not require any anesthesia. The embryos, now contained within a transfer catheter, are placed into the upper part of the uterus.
-
Step 6. Luteal Phase Support
-
In order to prepare the uterus for embryo implantation, progesterone medication is started on the day of or after egg retrieval. Progesterone is continued on a daily basis until the pregnancy is well into the 1st trimester.
-
-
Step 7. Early Pregnancy Surveillance
-
The first pregnancy test (termed a quantitative beta-hCG or simply, “a beta”) is performed 9-11 days after the embryo transfer. An average value is around 100 IU/L. hCG levels are monitored frequently during the first two of weeks of pregnancy after which point surveillance switches to ultrasound. By the 6th week of pregnancy, a fetus and heartbeat is typically visible.
risks and complications
IVF is a safe and common procedure. However, as with any medical intervention, there are a known number of risks associated with it. Ovarian hyperstimulation syndrome (OHSS) is a complication of using fertility medications and is characterized by varying degrees of electrolyte imbalance and fluid retention around the body. The mild form is common and presents with symptoms such as bloating or abdominal cramping. More severe forms are much less common but can be associated with potentially serious conditions such as blood clots or fluid retention around the lungs.
The egg retrieval itself is a surgical procedure and carries a risk of: 1) unanticipated bleeding leading to a blood transfusion or more invasive surgery 2) incidental damage to adjacent organs such as the bowel or bladder 3) infection and 4) anesthesia complications.
Finally, IVF is associated with an increased incidence of multiple gestations. The chance of having twins from an IVF cycle is approximately 30% in younger women and decreases with age. Triplets or higher order multiples occur in 2% of all IVF cycles.
For more information about our in vitro fertilization program, please contact us at 707.259.1955 or info@napavalleyfertility.com.