infertility basics
For those considering treatment, educating yourself about the fundamental concepts involved in reproduction and the basic approach to an infertility investigation is a logical place to start.
infertility basics
For those considering treatment, educating yourself about the fundamental concepts involved in reproduction and the basic approach to an infertility investigation is a logical place to start.
our biology
The Menstrual Cycle and Ovulation
The menstrual cycle is the end result of a highly complex and coordinated hormonal system involving the brain, the ovaries and the uterus. We commonly think of the cycle as lasting 4 weeks and being divided into two parts.
During the first half of a menstrual cycle, hormones from the brain signal the ovary to develop a single egg. When that egg has reached maturity (typically about day 14 of a 28 day cycle), a different hormone signal from the brain induces ovulation, the process whereby the egg is released from the ovary.
The second half of a menstrual cycle consists of the production of ovarian hormones which signal the uterus to get ready to support a pregnancy. If no pregnancy occurs, menstrual bleeding ensues and the cycle starts over.
Menstrual cycles can vary anywhere from 21 to 35 days in length. Cycle lengths outside this range suggest that ovulation is not taking place. Common conditions associated with anovulation include stress, intensive exercise and obesity or extreme thinness.
Male Hormones and Sperm Production
Just as with the female, the male reproductive system is under the control of hormone interactions between the brain and the gonads. Sperm maturation takes approximately 72 days to complete and it is estimated that men produce between 100-200 million new sperm each day.
Testosterone, the chief male hormone, is produced by the testes and is critical to healthy sperm production. Additionally, several specialized anatomic components of the male reproductive system such as the epididymis and seminal vesicles allow the sperm to go through their final maturation process.
Decreased sperm production can be the result of hormone imbalances, anatomical problems or environmental insults.
Female Age
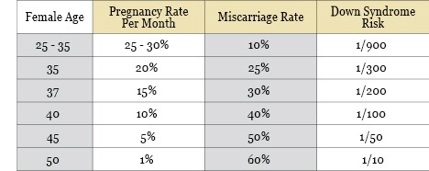
Women are born with a finite supply of eggs in their ovaries. With age, this number decreases naturally so that, by the time a woman reaches her late 40’s, almost all of her eggs have been depleted.
A diminishing number of eggs overtime results in not only a loss of quantity but also of quality. The end result is that becoming pregnant and giving birth to a healthy child is more difficult with age. The following table demonstrates the effect of female age on fertility:
reproduction 101
For normal reproduction to occur, the following events have to be fulfilled:
1) The female partner must be able to ovulate (release an egg from the ovary).
2) The ovulated egg must be healthy.
3) The male partner must be able to have an erection and ejaculate inside a woman’s vagina during sexual intercourse.
4) The ejaculate must contain an adequate number of healthy sperm.
5) The sperm must be able to travel from the vagina to meet the egg in one of the woman’s fallopian tubes.
6) The sperm must be able to fertilize the egg.
7) An embryo must develop, travel from the fallopian tube to the uterus and then implant into the uterine lining.
8) The ovary must produce a sufficient amount of hormones to support the pregnancy.
A problem involving any one of these steps can result in the inability to conceive.
Customarily, infertility is defined as no conception after 12 months of unprotected intercourse. For women over 35 years old, this time interval is shortened to 6 months, and for those over 40 years old, it is suggested that consultation with a fertility specialist is made as soon as conception is desired.
It is important to note that many individuals that meet the above definitions are not infertile but, rather, subfertile. That is to say, they are able to eventually conceive but may require a bit more time than average or the assistance of medical intervention. True infertility is a diagnosis reserved for individuals with almost no chance for pregnancy without therapy.
fertility testing
For the purposes of an investigation, we focus on the following three components of reproduction:
‣Female pelvic anatomy
‣Eggs
‣Sperm
1) Female Pelvic Anatomy (Uterus and Fallopian Tubes)
In order for pregnancy to occur, the uterus must be healthy and the fallopian tubes (used to transport sperm, eggs and embryos) need to be open and functional. These structures can be evaluated with the following tests:
Ultrasound: An ultrasound is imaging study performed in the office setting. Using sound waves to generate images on a viewing monitor, an ultrasound can document the size, shape, orientation and consistency of the uterus. Pathologies such as fibroids or polyps can also be detected.
Hysterosalpingogram (HSG): A hysterosalpingogram is an X-ray study performed in the outpatient hospital setting where radio-opaque dye is injected into the uterus. Dye outlines the contour of the endometrial cavity (inside of the uterus) and flows through the fallopian tubes. This helps define the anatomy of the uterus and demonstrate functionality of the tubes.
2) Eggs
Ovulation
In order for conception to occur, an egg must be released from the ovary. This process is known as ovulation and occurs, in most women, on a monthly basis. One of the simplest ways to confirm that ovulaton is taking place is to record monthly menstrual cycle symptoms in a diary. Mid-cycle pelvic discomfort, changes in cervical mucus and premenstrual symptoms all suggest normal ovulation. Other modalities to confirm ovulation include:
‣Basal body temperature charting
‣Ovulation predictor kits
‣Measurement of serum progesterone
‣Ultrasound
Egg Quantity and Quality
Women are born with a finite supply of eggs and, with age, the quantity and quality of the eggs diminishes. At any point in time, we are able to estimate how many quality eggs remain and we refer to this value as the “ovarian reserve”. Ovarian reserve can be estimated by performing the following tests:
‣Antral Follicle Count (AFC): This is an ultrasound assessment of the number of visible follicles (cystic structures in the ovary that each contain an individual egg).
‣Hormone Measurements
3) Sperm
Evaluation of the male partner is made with the semen analysis. A semen analysis is a microscopic assessment of individual sperm characteristics including their:
‣Number
‣Movement pattern
‣Shape
These values are used to predict adequacy for conception. In the event that an abnormality is discovered, further testing in the form of a repeat semen analysis or hormone measurements may be ordered.
Following the completion of the above evaluations, a treatment plan is formulated. If there are identifiable problems, therapy will focus on these. In the situation where all testing is normal (known as “unexplained infertility”) treatment is started empirically.
For more information about fertility basics, please refer to our page of FAQs or contact us at 707.259.1955 or info@napavalleyfertility.com
Napa Valley Fertility Center provides highly-attentive reproductive medicine and expertise in all aspects of infertility care. These include: in vitro fertilization (IVF), intrauterine insemination (IUI), ovulation induction, frozen embryo transfer, third party reproduction, male infertility/andrology, pre-implantation genetic diagnosis, and reproductive surgery. We also emphasize access to experimental treatments such as in vitro maturation (IVM) and offer fertility preservation therapies for women with cancer or benign conditions that threaten their reproductive lifespan. Dr. Peter Uzelac, our physician and medical director, is certified by the American Board of Obstetrics and Gynecology in Reproductive Endocrinology and Infertility. He is also a member of the Society for Reproductive Endocrinology and Infertility (SREI). Dr. Uzelac launched one of the first successful IVM programs in the United States.
©2010-2012 Napa Valley Fertility Center. All rights reserved.